The corona pandemic laid bare the terrible state of our public health system. Even the godi media was forced to acknowledge the crisis, as the social media was full of news about people desperately searching for hospital beds, oxygen, medical supplies for their loved ones … people were dying like flies, there was no place in the crematoriums, bodies were floating down the Ganges …
While India officially reported 4.8 lakh deaths from SARS-CoV-2 infections as at the end of 2021, several studies have estimated that the actual death rate was at least six to seven times higher. In May 2022, the WHO released a report that estimated that there were 47.4 lakh excess deaths in India during the pandemic years 2020–21.[1] Several other research groups have also put out estimates of India’s pandemic deaths, which range from between 30 to 50 lakh deaths. This implies that India accounted for nearly a third of pandemic deaths globally.[2]
But actually, India was facing a ‘health emergency’ even before the corona pandemic struck the country in early 2020. Lakhs of people die every year of entirely curable diseases. TB alone kills more than 3 lakh people every year, 2 deaths every 3 minutes — this is more than the number of official deaths due to Covid.[3] India is known as the Chronic Heart Disease (CVD) capital of the world — CVD is now responsible for a quarter of all deaths in the country.[4] Even worse: 1.2 lakh children under the age of five die every year of diarrhoea — a disease for which there is a simple treatment solution.[5] The reason why these deaths do not make media headlines is that it is the poor who the worst sufferers of this health crisis. But the corona hit everyone, including the rich, and so this crisis could not be brushed under the carpet.
The reason why our health system is in ICU is India’s extremely low level of public health spending.
Modi Government’s Public Health Expenditure
Domestic general government expenditure on health in the developed countries of the OECD is around 8.7 percent of GDP. For the countries of the European Union, this figure is 8.4 percent of GDP. The governments of the countries of Latin America and the Caribbean spend an average of 4.4 percent of GDP on providing healthcare to their citizens. Government spending on health in Brazil is 4.5 percent of GDP, Mexico 3.1 percent, Russia 5.3 percent, South Africa 5 percent and Turkiye 3.6 percent (all figures for 2021). The world average is 6.5 percent (Chart 11.1).
Chart 11.1: Domestic Government Expenditure on Health as % of GDP [6]
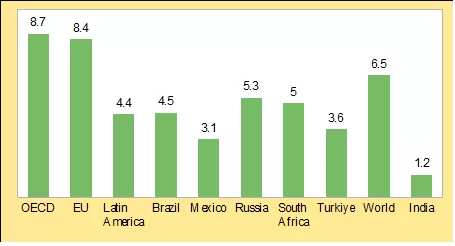
In contrast, India’s public health spending is abysmally low. According to the WHO and World Bank, India’s general government (Centre + States) spending on health has been just around 0.9 to 1.2 percent of GDP in recent years.[7] The Modi Government’s Draft National Health Policy of 2015 too admitted that India’s public health spending was just 1.04 percent of GDP.[8] The Economic Survey 2020–21 makes an even more frank admission: “India ranks 179th out of 189 countries in prioritisation accorded to health in its government budgets (consolidated Union & State government)”. It further says: “on quality and access of healthcare, India was ranked 145th out of 180 countries.[9]
The difference between public health expenditure of developed countries and India becomes starker when we compare per capita government expenditure on health. The per capita domestic government health expenditure in the developed countries is as high as $3,692. For countries of Latin America and the Caribbean, it is $349. The world average is $797. In contrast, India’s per capita public health spending is abysmally low — the WHO / World Bank reckon it to be a lowly $25 (all data for 2021).[10]
The Modi Government’s National Health Policy (NHP)
During the 2014 Lok Sabha election campaign, the BJP promised to accord “high priority” to the health sector if voted to power, and promised a universal health assurance plan. Soon after coming to power in 2014, it released a Draft National Health Policy. In its opening paragraph, the draft frankly acknowledges that India’s healthcare services are in a dismal state: “much of the ill health, disease, premature death, and suffering we see on such a large scale is needless, given the availability of effective and affordable interventions for prevention and treatment.”[11] It attributes this crisis to India’s low level of public health spending: “The failure to attain minimum levels of public health expenditure remains the single most important constraint. While it is important to recognise the growth and potential of a rapidly expanding private sector, international experience shows that health outcomes and financial protection are closely related to absolute and relative levels of public health expenditure…. Global evidence on health spending shows that unless a country spends at least 5–6 percent of its GDP on health and the major part of it is from government expenditure, basic healthcare needs are seldom met. The government spending on healthcare in India is only 1.04 percent of GDP …” [12]
The Draft NHP set a target of increasing the country’s public health expenditure to 2.5 percent of GDP. It stated that though “a full achievement of the goals and principles as defined would require an increased public health expenditure to 4 to 5 percent of the GDP”, but given the limited financial capacity of the country, “this policy proposes a potentially achievable target of raising public health expenditure to 2.5 percent of the GDP. It also notes that 40 percent of this would need to come from Central expenditures.” It proposed a timeline of five years for achieving this target. [13]
But after its release, the draft was put in cold storage for more than 2 years. It was probably prepared by some over-enthusiastic bureaucrats, and according to newsreports, PM Modi and his team were not happy with the financial implications of the policy and the primacy accorded to public health services, and so delayed finalising it. The matter even reached the Supreme Court which asked the Central Government in September 2016 to take a final call by December 31 on whether it would like to frame a National Health Policy or not.[14]
Note that the target set in the Draft NHP for total public health spending of 2.5 percent of GDP was less than half the average global public health expenditure (6.5 percent). Nevertheless, the Modi Government dilly-dallied for more than 2 years on committing itself to such a modest increase in its health expenditure.
The National Health Policy was finally given approval by the Union Cabinet in March 2017. It reiterated the target mentioned in the Draft NHP of increasing “health expenditure by government as a percentage of GDP from the existing 1.15 percent to 2.5 percent”, but extended the time frame to achieve this modest goal to 2025. NHP-2017 also proposes that the States increase their health spending to more than 8 percent of their budgets by 2020.[15]
The draft NHP had proposed that the Centre spend 40 percent of the health spending target of 2.5 percent of GDP. The NHP is silent on this issue. But PM Modi has announced innumerable times that his government “is committed to ensuring accessible, affordable, and top-quality healthcare for every Indian”,[16] is committed “to ensure that everyone is healthy and healthcare is affordable”,[17] that “making medical treatment affordable has been the top-most priority of our government”.[18] One of the most essential conditions for fulfilling this promise is that the Centre increases its health spending — to at least 1 percent of GDP, which is actually a very moderate target. The NHP set a deadline of 2025 to increase health spending to 2.5 percent of GDP. Therefore, in this article, we measure the seriousness of PM Modi’s promise of providing affordable healthcare for all by examining the progress made by the Centre in increasing its health spending to reach 1 percent of GDP by 2025.
Actual Health Spending During Modi Years
The Modi Government made it clear in its very first year in office that health spending was not going to be one of its priority areas. It slashed the budgetary allocation on health (by this we mean the combined allocation for Ministry of Health and Family Welfare and Ministry of AYUSH) from the 2014–15 budget estimate of Rs. 39,237 crore to Rs. 32,154 in 2014–15 Actuals, a cut of nearly 20 percent.
Since then, the Centre’s health spending has steadily increased to Rs. 94,671 crore in this year’s budget estimate (Chart 11.2). On the face of it, this appears to be a significant increase. The Modi Government has cited this increase to counter criticism by the medical journal Lancet about India’s declining public health expenditure.[19]
Chart 11.2: Total Spending on Health, FY15–FY25 (Rs. crore)
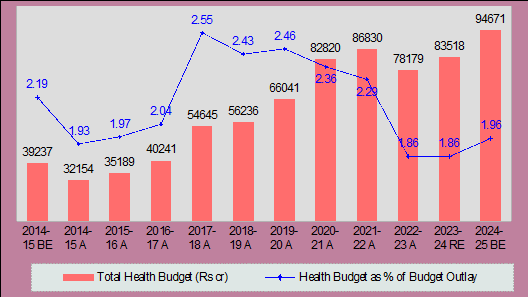
Health Budget = Budget allocation for Ministry of Health and Family Welfare + Ministry of AYUSH
The problem with this rebuttal is that the government is citing nominal figures. A better idea of the Modi Government’s prioritisation of healthcare is obtained by comparing its health budget outlay to its total budgetary spending, or to GDP. In Chart 11.2, we present the health budget as a percentage of total budget expenditure. The chart shows that this peaked in 2017–18 A (2.55 percent), the year NHP-2017 was released, after which it has steadily declined to 1.96 percent this year, a fall of 23 percent. The reduction has been so steep that health spending as a percentage of total budget expenditure this year (2024–25 BE) is less than in 2015–16 (1.97 percent).
In Chart 11.3, we plot the Centre’s total health spending as a percentage of GDP. This too has steadily fallen after reaching a peak of 0.42 percent of GDP in 2020–21 A. This year’s allocation (0.29 percent) is 30 percent below the 2020–21 level, which means it is less than one-third of the target of 1 percent of GDP. It is even below the level of 2017–18 (0.32 percent), the year NHP was released. This only means that the Modi Government is simply not interested in implementing the financial target set out in NHP-2017. That too has turned out to be a JUMLA.
Chart 11.3: Total Health Spending of Centre as % of GDP, FY15–FY25
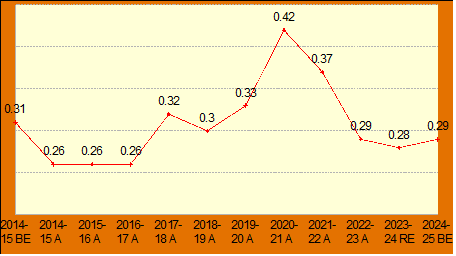
* Total Health Budget of Centre = Budget allocation for
Ministry of Health and Family Welfare + Ministry of AYUSH
As we have discussed in a previous article of this budget series, the Constitution tasks the States to undertake most of the welfare-related expenditures (including health spending), but the Centre collects the bulk of the revenues in the country. To check this imbalance, the Constitution provides that the Centre must transfer a part of its revenues to the States. But the Modi Government, in violation of the country’s federal structure, has been resorting to all kinds of tricks to reduce its transfers to the States. This has adversely affected social sector spending of the States, including their health sector spending. So, while the NHP calls upon the States to increase their health spending to 8 percent of their total spending, this has fallen from the peak of 5.9 percent reached during the Covid year 2021–22 A to 5.6 percent of their total budget expenditure in 2023–24 BE.[20]
Consequently, in the ten budgets presented during Modi’s first two terms, India’s total public health expenditure (Centre and States combined) has hovered at a lowly 1 to 1.2 percent of GDP.[21] Recently, The Lancet, one of the most prestigious health journals in the world, also pointed out in an editorial that:
“Health care under Modi has fared poorly… Overall, government spending on health (in India) has fallen and now hovers around an abysmal 1.2 percent of gross domestic product.”[22]
State of India’s Public Health Services
The result of this low government spending on health is that India’s public health services are in a dismal state.
Modi’s Health Jumla: Health and Wellness Centres
In rural India, the structure of the public healthcare system is a 3-tier system consisting of health sub-centres (HSCs), primary health centres (PHCs) and community health centres (CHCs).
Soon after the release of the NHP-2017, FM Arun Jaitley announced in his 2018 budget speech a plan to upgrade all the 1.5 lakh health sub-centres (HSCs) in rural areas into Health and Wellness Centres (HWCs). He stated, “These centres will provide comprehensive health care, including for non-communicable diseases and maternal and child health services. These centres will also provide free essential drugs and diagnostic services. I am committing Rs. 1,200 crore in this budget for this flagship programme.”
The budget for upgrading HSCs into HWCs comes under the budget sub-head National Rural Health Mission (NRHM). The NRHM is the overarching program of the Centre to provide accessible and quality healthcare to the rural population. Table 11.1 gives the budget spending on HWCs for the four years after their announcement (2017–18 to 2021–22). [After the 2021–22 budget, we do not have any idea of the Modi Government’s budgetary spending on NRHM or HWCs, as the budget for NRHM has been merged into the budget for National Health Mission (NHM).] The table shows that while the finance minister did increase the spending on HWCs by an annual average of 18 percent over this four-year period for which data is available, the budget allocation for NRHM increased only marginally — by an average of only 1.2 percent per year over these four years, implying a decrease in real terms. This means that while the FM reduced the total budgetary spending on our rural health services, he reshuffled the spending being done under various heads to show an increase in spending under HWCs.
Table 11.1: Budget Allocation for NRHM and HWCs, FY18–FY22 (Rs. crore)
| 2017–18 A | 2018–19 A | 2019–20 A | 2020–21 A | 2021–22 A | Average Annual Increase | |
| HWCs | 993 | 1,145 | 1,347 | 1,548 | ||
| HWCs: Increase over previous year | 45.5% | –6.8% | 14.9% | 17.9% | ||
| NRHM | 26,178 | 25,495 | 29,987 | 30,329 | 26,945 | |
| NHRM: Increase over previous year | –2.6% | 17.6% | 1.1% | –11.2% | 1.2% |
State of Rural Health Services
What is the state of our HSCs, now grandiosely renamed as Health and Wellness Centres? The recently released Rural Health Statistics 2021–22 (RHS) gives data on the state of rural health infrastructure and workforce in the country. The figures given therein are shocking: there is a 25 percent shortfall in the number of HSCs (or HWCs!), 31 percent in PHCs and 64 percent in CHCs in the country, as compared to the IPHS norms of population to health facilities (see Table 11.2). Indian Public Health Standards (IPHS) are essential benchmarks set out by the Government of India that the public health system should strive to achieve.[23]
Table 11.2: State of Rural Health Infrastructure, 2022 [24]
| HSCs | PHCs | CHCs | |
| Required [as of March 2022] (1) | 1,93,310 | 31,640 | 7,894 |
| Functioning | 1,57,935 | 24,935 | 5,480 |
| Shortfall‡ (2) | 48,060 (25%)* | 9,742 (31%)* | 2,852 (64%)* |
‡ All India shortfall is derived by adding state-wise figures of shortfall ignoring the existing surplus in some states.
* Figure in brackets: Shortfall in all States as a percentage of required health centres; calculated as [(2) / (1)] x 100
Even the functioning rural health centres are in a terrible state. According to the RHS 2021–22 report, the HSCs, PHCs and CHCs suffer from a severe shortage of doctors, nurses and other staff, as compared to the minimum numbers mandated by IPHS standards. We give some of these shortfalls in Table 11.3.
Table 11.3: Status of Health Manpower in Rural Health Centres, 2022 [25]
| Required | Shortfall | Shortfall as % of Required | ||
| HSCs | Health Worker (Female) / ANM | 1,57,935 | 8,208 | 5.2% |
| HSCs | Health Worker (Male) | 1,57,935 | 1,05,244 | |
| PHCs | Doctors | 24,935 | 776 | 3.1% |
| PHCs | Health Assistants | 49,870 | 36,981 | |
| PHCs | Laboratory Technicians | 24,935 | 1,0434 | |
| PHCs | Nursing Staff | 24,935 | 4,211 | |
| CHCs | Total Specialist Doctors | 21,920 | 17,435 | 79.5% |
| CHCs | General Duty Medical Officers (Allopathic) | 10,960 | 372 | |
| CHCs | Radiographers | 5,480 | 3,206 | |
| CHCs | Nursing Staff | 38,360 | 1,591 |
- In the rural areas, the main hospital is the CHC. It is supposed to have 4 specialist doctors — surgeon, physician, gynecologist/obstetrician and pediatrician. Only one-third of the required number of CHCs are functioning, and even these suffer from a 80 percent shortage of doctors.
- A PHC is to be manned by a medical officer supported by paramedical and other staff (including at least 2 health assistants and 1 nurse). Only 69 percent of the PHCs are operational, and these too suffer from a 3.1 percent shortage of doctors, 75 percent shortage of health assistants, and 17 percent shortage of nursing staff.
- Each HSC is supposed to be staffed by at least one auxiliary nurse midwife (ANM) / female health worker and one male health worker. The IPHS norms were first published in February 2007; even after 17 years, there exists a 25 percent shortfall in the required number of HSCs. And of the HSCs functioning, majority do not have the required staff of one auxiliary nurse midwife (ANM) / female health worker and one male health worker.
A significant number of the HSCs and PHCs in several states do not even have water supply and electricity:
- 3.7 percent PHCs do not have electric supply; 5 percent of the PHCs do not have water supply; and 7.9 percent of the PHCs do not have an all-weather motorable approach road.
- 11.4 percent HSCs (17,967) do not electricity supply, and 9.5 percent (14,935) do not have regular water supply.[26]
How does a health centre function without electricity and regular water supply?
The overwhelming majority of our rural health centres are thus not functioning as per government mandated or IPHS guidelines. The Modi Government has resorted to concealing this data too; the latest RHS 2021–22 is silent about this. The RHS 2019–20 is the last report to give this statistic — according to it, as of March 2020, only 8.5 percent CHCs, 13.2 percent PHCs and 3.5 percent HSCs were functioning as per IPHS norms (see Table 11.4). The data given in Table 11.1 shows that over the period 2019–20 to 2021–22, the budget for NRHM declined in real terms. Therefore, the condition of our rural health infrastructure and human resources cannot have significantly improved over these two years. Hence, we can assume that in 2021–22, the percentage of our rural health centres functioning as per IPHS guidelines must be nearly the same as in 2019–20. This means that in 2021–22, only 5,500 of the more than 1.5 lakh HSCs, 3,300 of the 25,000 PHCs and 466 of the 5,500 CHCs in the country were functioning as per IPHS standards (see Table 11.4).
Table 11.4: Rural Health Centres Functioning As Per IPHS Guidelines, 2022 [27]
| HSCs | PHCs | CHCs | |
| Functioning (1) | 1,57,935 | 24,935 | 5,480 |
| % of health centres functioning as per IPHS guidelines in 2019–20 (2) | 3.5% | 13.2% | 8.5% |
| Total health centres functioning as per IPHS guidelines in 2021–22† | 5,527 | 3,291 | 466 |
† We assume that this percentage is the same as in RHS 2019–20. Calculated as: [(1) x (2)] / 100
And yet, in December 2022, the Ministry of Health and Family Welfare claimed in a press statement that the target of setting up 1.5 lakh HWCs across the country had been achieved.[28] The Modi Government has conjured up these HWCs without spending a penny.
That most of the HWCs exist only on paper is also borne out by several newsreports.[29]
The Modi Government is too thick-skinned to be bothered about such pinpricks. In 2023, it rechristened the Ayushman Bharat-Health and Wellness Centres as ‘Ayushman Arogya Mandirs’.[30]
State of Urban Primary Health Services
After independence, the focus of India’s public health policy was on providing health facilities in rural areas as they were virtually non-existent. Consequently, primary urban health infrastructure remained neglected. In 2013, the UPA Government launched the National Urban Health Mission (NUHM) to provide equitable and quality health services in urban areas with a special focus on slums. Under this, urban PHCs and CHCs were to be set up. While approving the NUHM in 2013, the Union Cabinet had estimated its cost for five years to be Rs. 22,507 crore, of which the Centre undertook to provide 75 percent or Rs. 16,955 crore (which works out to around Rs. 3,400 crore per annum).[31]
The very next year, the Modi Government came to power, and from its very first year, it neglected the NUHM. The allocation for this program in the Union Budget has remained way below the amount committed at the time of its launch — the average allocation over the 8-year period 2014–15 to 2021–22 is only Rs. 684 crore, less than 20 percent of the proposed Central allocation (see Chart 11.4). [After 2021–22, we don’t have any idea about the allocation for NUHM, as it has been merged into the budget for NHM.]
Chart 11.4: Budget Allocations for NUHM, FY15–FY22 (Rs. crore) [32]

Consequently, the urban PHCs and CHCs too suffer from a severe shortage of doctors and paramedical staff (see Table 11.5). The latest data we have is for 2022.
Table 11.5: Status of Health Manpower in Urban Health Centres, 2022 [33]
| Required | Shortfall | |||
| Total Number of PHCs | Total Number of PHCs | 9,618 | 3,822 | |
| PHCs | Doctors | 6,118 | 308 | 5% |
| PHCs | Health Workers | 30,590 | 10,864 | |
| PHCs | Laboratory Technicians | 6,118 | 1,780 | |
| PHCs | Nursing Staff | 6,118 | 71 | |
| CHCs | Total Specialist Doctors | 2,336 | 1,097 | 47% |
| CHCs | General Duty Medical Officers (Allopathic) | 1,168 | 172 | |
| CHCs | Radiographers | 584 | 288 | |
| CHCs | Nursing Staff | 4,088 | 216 | |
- There is a 40 percent shortfall in the required number of urban PHCs;
- The functioning PHCs suffer from a 5 percent shortage of doctors and 35.5 percent shortage of Health Workers (Female) / ANMs;
- The urban CHCs suffer from a 47 percent shortage of specialist doctors.
Tertiary Facilities
According to the National Health Profile released in 2023, there are a total number of 8.49 lakh hospital beds in government hospitals in the country (63% of these are in urban areas).[34] This works out to 0.62 public hospital beds per 1000 population.[35] Including private hospitals, this figure increases to 1.3 hospital beds per 1000 population. This is way below the WHO recommended 3 beds per 1000 population.[36] Even if we assume that at least 50 percent of the deficit should come from the public sector, that means there is a shortage of 11.7 lakh beds at the minimum in government hospitals.[37]
With such a massive shortage of doctors, auxiliary hospital staff and health infrastructural facilities, in both the primary health services and tertiary care services, no wonder the pandemic completely overwhelmed our country’s public health system.
Modi Government’s Health Priorities
Let us now analyse the government’s health priorities (that is, the actual health policy of the Modi Government), by examining the allocations for various schemes in the health budget.
The NRHM and NUHM are the most important Central schemes for ensuring availability of primary healthcare in rural and urban areas. While both are sub-missions of the National Health Mission (NHM), till 2022, separate allocations were made for both these schemes in the health budget. From the 2022–23 budget onwards, for reasons best known to the Health Minister / FM, the allocations for these schemes have been merged into the budget for NHM, and we now have only the total allocation for NHM in the budget papers.
We make an estimate of the total budget allocation for improvement of primary healthcare in the rural and urban areas (we call this Primary Health Services Budget or PHSB), from the NHM budget, by deducting from it the allocations for building / upgrading District and State hospitals made in the NHM budget.[38] In Chart 11.5, we compare this to the budget allocation for building new elite government hospitals.[39]
The overall concern of the Modi Government towards strengthening primary healthcare can be inferred from the share of primary health services budget (PHSB) in the total health budget as shown in Chart 11.5. The budget allocation for PHSB has declined from 58 percent of the total health budget in 2014–15 to 40 percent in this year’s budget — a fall by 18 percentage points.
On the other hand, the total budget for building new hospitals has risen steeply in the successive Modi budgets from 2.4 percent of the total health budget in 2014–15 to 16.5 percent in 2021–22 before declining to 10.9 percent this year. Of this, nearly 70 percent is for building new AIIMS. This year, within the allocation for building hospitals of Rs. 10,275 crore, Rs. 6,800 crore is for establishing new AIIMS.
Chart 11.5: Primary Health Services Budget vs Allocation for Building Hospitals , FY15–FY25 [40]
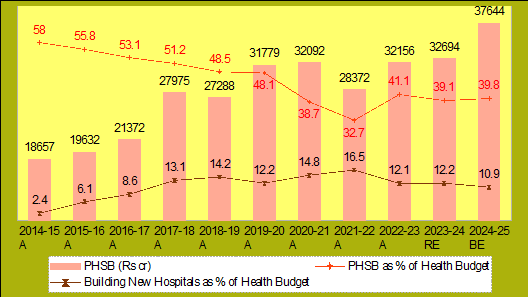
Primary Health Services Budget (PHSB) includes: NHM in Health and Family Welfare + NHM in AYUSH – budget for ‘Human Resources for Health and Medical Education’ (where it is included in the NHM budget).
Budget for Building Hospitals includes: ‘Pradhan Mantri Swasthya Suraksha Yojana’ + ‘Human Resources for Health and Medical Education’ + ‘Establishment Expenditure of New AIIMS’.
Health Budget includes: Ministry of Health and Family Welfare + Ministry of AYUSH.
What is the point in building high quality AIIMS, without strengthening the primary healthcare centres — the HSCs, PHCs and CHCs — the basic health units of our rural and urban health system, which are suffering from a severe shortage of infrastructure and trained medical personnel?
This does not mean that new high quality public tertiary hospitals are not needed — the problem is that this is being done while the primary healthcare sector is being neglected. If funds are limited, then priority should be given to improving the primary health services (and actually, as we show in a later article, if the government so desires, it can increase its revenues and spend it on improving both primary health services as well as building new hospitals). If primary level health services are good — that is, if the HSCs, PHCs and CHCs are running well — most illnesses can be taken care of at this level itself. It will reduce the load on the tertiary hospitals. This will not only improve the efficiency and reduce the cost of delivery of public health services, it will also improve the overall health status of the people. Therefore, priority should be given to improving primary healthcare.[40] But in the Modi Government’s ‘Idea of India’, the poor don’t exist.
Such is the incompetence / misgovernance of the Modi Government that despite the allocation of thousands of crores of rupees, the construction of new AIIMS has stalled. The footnote to the 2024–25 budget document of the ‘Department of Health and Family Welfare’ says that so far, under Pradhan Mantri Swasthya Suraksha Yojana (PMSSY), approval has been granted for establishing 22 new All India Institute of Medical Sciences (AIIMS). It further claims that 6 of these AIIMS — in Bhopal, Bhubaneswar, Jodhpur, Patna, Raipur and Rishikesh — conceptualised during the Vajpayee government tenure are “fully functional”. But with regard to the remaining 16 AIIMS that have been announced by the Modi Government after it came to power in 2014, the document does not use the term “fully functional” for any of them. It only says that 11 of these are “functional”, including the 4 AIIMS announced way back in 2014! They are offering only limited OPD and IPD services. A report in The Wire points out that even the 6 AIIMS announced by the Modi Government as fully functional do not have full staff strength — in some of them, only 50 percent of the faculty posts sanctioned have been filled, and the shortage of non-faculty staff is even worse.[41]
Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (PM-JAY)
This is the most hyped health scheme of the Modi Government. When he announced this scheme in his budget speech in 2018, the then Finance Minister Arun Jaitley proclaimed it as “the world’s largest government funded health care programme”. Under this scheme, the government promised to provide medical insurance cover of Rs. 5 lakh per family to 10 crore poor families (roughly 50 crore people). In January 2022, the Union government expanded the coverage to 12 crore families based on NFSA data, equivalent to roughly 55 crore people. As per a Ministry of Health press release, as of 30 June, 34.7 crore health cards had been created under this scheme in the country.[42]
The godi media has exuberantly described this scheme as a universal healthcare scheme, that fulfills the promises made by our dear PM on providing “accessible, affordable, and top-quality healthcare” to all Indians. But it is an absolute lie. This scheme does not provide universal healthcare, it is only a hospitalisation insurance scheme! It does not cover outpatient costs, and these constitute more than two-thirds (68 percent) of the health related out-of-pocket expenditure or OOPE (that is, personal spending by people) in India.[43]
Furthermore, the financial allocation for this scheme is not enough to cover the hospitalisation insurance costs of all the poor in India. A 15th Finance Commission report estimated that total costs for PM-JAY in 2019, taking then levels of hospitalisation rates and expenditure and assuming full coverage, would range between Rs. 28,000 crore and Rs. 74,000 crore, with projections for 2023 being more than double this range.[44] But the budgetary allocation for this scheme has been less than a quarter of the lower end of this estimate in all the budgets so far; and even this low allocation has never been fully spent (see Chart 11.6). This only means that the Modi Government is not serious about providing even limited healthcare to all our people.
Chart 11.6: Budget Allocation and Actual Spending for PM-JAY (Rs. crore)
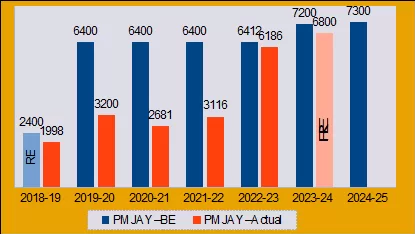
For 2018–19, there was no allocation in the BE, only in the RE. For 2023–24, we do not have the actual figures as yet, so we have given the RE.
Even this inadequate spending is being siphoned off by racketeers. In 2023, CAG investigated PM-JAY and its report shows that the scheme is marred with large-scale corruption. The auditor found several irregularities, from treating dummy patients to providing purported treatment after the patient had died.[45]
But more than corruption, the bigger problem with this scheme is that it depends on private hospitals to provide healthcare to people. Private hospitals are essentially businesses whose sole aim is to maximise their profits. Apart from a few high-quality but very costly private corporate hospitals, the others only fleece patients without even providing them decent healthcare. This is also admitted by the Economic Survey 2020–21. It says that even though costs of treatment are “uniformly higher in the private sector”, “quality of treatment does not seem to be markedly better in the private sector when compared to the public sector.”[46]
If private hospitals do not provide better quality healthcare than public hospitals, but are much more costly, and this is a conclusion drawn by the government’s own economic advisors, then why is the government pushing for an insurance scheme to treat the poor in private hospitals? Why is it not increasing public health expenditure to improve public hospitals so that people can be treated there at much cheaper rates? This is also the precise recommendation of the 2023 CAG report mentioned above: “There is a strong need to invest in public hospitals to improve and upgrade the quality of the existing health facilities …”[47]
This is actually simple economics common sense. If the Modi Government is not increasing its public health expenditure to improve the quality of our public health services, then it can mean only one thing — that the Modi Government is not really concerned with providing cost-efficient good quality healthcare to all our people, especially the poor. The real purpose behind PM-JAY is to privatise healthcare and transform this sector into an opportunity for profit-making by private businesses. The CEO of the PM-JAY scheme himself sent out a tweet encouraging private hospitals to get themselves empanelled with the scheme: “We are offering you business of 50 crore people!”[48]
As a part of this push to privatise healthcare, the Centre has announced incentives for the private sector to set up hospitals in Tier 2 and Tier 3 cities, to the extent of providing them grants (not loans!) of up to 40 percent of the total cost of the project! As if this is not enough, the Niti Aayog and the health ministry have also recommended to all States that they partially privatise their district hospitals.[49]
So, under the cover of the “world’s largest healthcare initiative”, the Modi Government is destroying whatever little that remains of India’s failing public healthcare system, and privatising it.
Making Sense of the Decline in OOPE
But then how does one explain recent data from National Health Accounts (NHA) that claims that share of government health expenditure in total health expenditure of India has increased from 29 percent in 2014–15 to 41.4 percent in 2019–20, and out-of-pocket expenditure (OOPE) of people has nosedived from 62.6 percent of total health expenditure in 2014–15 to 47.1 percent in 2019–20.[50] The Modi Government and its hanger-on godi media have been celebrating this as proof of the Modi Government’s commitment to ensuring the provision of affordable quality health facilities to citizens.
Firstly, even an OOPE of near 50 percent is very high; it is among the highest in the world. WHO data for 2021 shows that even if we accept this government figure, India ranked 163 out of 190 countries in out-of-pocket expenditure.[51]
Secondly, one important question still remains. All the facts given above, all of which are from official sources — about Modi Government’s declining budgetary allocation for healthcare, the decline in health spending of States, the massive shortage of doctors and paramedical staff and health infrastructure in the rural and urban health centres, priority given to building elite hospitals instead of strengthening the primary healthcare system (and even these are not functional), the extremely inadequate spending on PM-JAY — unequivocally show that public investment on health during the Modi years has declined, and our public health services are in an abysmal state. The claim of the NHA, that the share of the government in total health expenditure of the country has increased by more than 12 percentage points during the Modi years, is therefore farcical! The Modi Government is manipulating data to show the healthcare situation in the country in a rosy light.
Two articles, one by Professor Indranil Mukhopadhyay of the Jindal School of Public Policy, and another by Mampi Bose, a faculty member at Azim Premji University, point to several anomalies in the data used by the NHA to show an increase in public investment on healthcare in India and a decline in OOPE.[52]
We briefly discuss here only one important argument made by Professor Indranil.
A key factor that NSS measures to determine access to healthcare is the rate of hospitalisation. NSS survey data show that in 2014, India had 37.1 hospitalisations for every 1,000 people. By 2017–18, the rate of hospitalisation had fallen to 28.2 — a decline of 24 percent. Further, the decline is more for the poorer quintile groups and STs residing in rural areas. This is the first time in four decades that hospitalisation rate has declined. The official interpretation of this data is that this shows an improvement in health of people because of better delivery of public health services. However, the experience of various developing countries indicates that as public spending on healthcare increases and quality of public health services improves, their utilization rates increase as people who earlier couldn’t afford healthcare and therefore did not visit hospitals now start accessing healthcare facilities. This means that the decline in hospitalisation rate and reduction in OOPE is an indicator of reduced healthcare utilisation, rather than increased government healthcare spending.
This is also borne out by recent data from National Family Health Survey-5 (2019–21) whose data was released in 2022. It reveals that approximately 60 percent of women in India cannot access affordable health services due to inadequate infrastructure and a shortage of healthcare workers. According to NFHS-5, 40.4 percent of women reported being unable to access medicines, and 39.2 percent could not reach healthcare providers.[53]
Therefore, the decline in OOPE is a sign of distress rather than a cause of celebration. Indranil also points to limitations with the NSS data based on which NHA has made its estimates, and draws attention to other data that show that OOPE may have actually increased over this period.[54]
Modi Government’s Actual Health Policy
On the basis of this detailed discussion, we can now draw conclusions regarding the actual health policy of the Modi Government:
- The NHP-2017 is only a smokescreen; it is only for publicity and seminars, where intellectuals and healthcare professionals with no concern for the health of our people go bonkers over it.
- Within its limited health budget, the Modi Government is reducing its expenditure on primary healthcare — despite the fact that in India’s vast countryside, our health facilities are in a dilapidated state, beset by lack of trained medical staff, dysfunctional equipment, lack of essential medicines, and even shuttered centres. At the same time, it is increasing the outlay for building new elite hospitals like AIIMS. This is in tune with the pretentious and elitist approach of the Modi Government — build a few high quality facilities amidst a huge expanse of neglect and ruin. This is what is happening in every sector — build a few airports, while neglecting basic transport infrastructure like the public bus transport system; build a bullet train, while undermining the railways; build a few IITs and PM-SHRI schools, while neglecting school and college education.
- A Niti Aayog report titled Investment Opportunities in India’s Healthcare Sector lays bare the agenda of the government. It says: “(T)here are nearly 600 investment opportunities worth USD 32 billion (INR 2.3 lakh crore) in the country’s hospital/medical infrastructure sub-sector.”[55]
This means that the Modi Government views the health sector as a sector for profit-making, in which business houses should invest and make profits. And so it is gradually reducing its budget outlay for health, privatising existing government hospitals, and encouraging the private sector to enter, takeover and dominate this sector. To facilitate the takeover of the healthcare sector by private hospitals, it has launched the PM-JAY scheme which is nothing but a scheme for transferring public funds to private hospitals.
Consequences for the People
India is facing a health emergency. The worst victims of this are the poor. It is not very long ago that bodies were floating down the Ganga — one only needs to recall those tragic visuals to be reminded of the terrible state of our public health system. But the thick-skinned Modi Government has learnt no lessons from that tragedy that had such catastrophic consequences for the people. Rather than increasing public investment in health and improving the country’s public health facilities, it is doing the opposite — it is reducing its investment on health, and accelerating privatisation of healthcare.
The Modi Government is an absolutely heartless government. Private healthcare is exceedingly costly. Because of lack of good quality public health facilities, when common people admit their loved ones in private hospitals in a desperate attempt to save their lives, these profit centres strip them to their bones. Even the Niti Aayog admitted in a 2021 report that high costs of health services in the private sector push 7.5 percent of India’s population — about 10 crore people — into poverty every year.[56]
But what about those who have nothing to mortgage in order to access private healthcare? They have no option but to depend on public health services, which are non-existent or in bad shape in several parts of the country, as the above statistics show. A study by global experts published in The Lancet, one of the world’s highest-impact academic journals, in 2018 found that some 24 lakh Indians die of treatable conditions every year — around 16 lakh die due to poor quality care, and 8 lakh die because they do not have access to healthcare. Of the 130 nations studied for the report, the death rate in India (deaths per 1 lakh population) due to poor quality healthcare was the worst; even our neighbours Pakistan, Nepal, Bangladesh and Sri Lanka fared better.[57]
Medical Tourism
The private corporate hospitals mushrooming in India’s big cities across the country need patients in large numbers to make profits. The overwhelming majority of India’s population just cannot afford the cost of treatment in these elite hospitals — they are even beyond the reach of India’s middle class. So, these hospitals are targeting rich patients from abroad.
The Modi Government, whose sole policy orientation is to promote the profits of the corporate houses, is helping them in this. It has even been given a name — ‘medical tourism’. The responsibility of promoting this has been delegated to the Ministry of Tourism (and not the Ministry of Health!). A report in the Times of India (a prominent godi newspaper) titled “Medical Tourism – How India Is Leading the Game” is effusive in its praise:
India has become a top player in medical tourism, offering affordable and high-quality healthcare. With visionary leaders, government support, and a skilled workforce, India attracts patients from around the world.[58]
A press release by the Ministry of Tourism says that the total Foreign Tourist Arrivals for medical purpose has zoomed during the past few years, going up from 1.83 lakh in 2020 to 6.35 lakh in 2023.[59]
While lakhs of people die every year in India because of lack of affordable healthcare facilities, the country is on its way to becoming a Medical Superpower too!
Notes
- “WHO Says 47 Lakh Excess Covid Deaths in India”, 6 May 2022, https://www.deccanherald.com.
- Ditsa Bhattacharya, “India’s COVID-19 Deaths 6–7 Times Higher Than Official Figures: Analysis”, 10 January 2022, https://www.newsclick.in; Murad Banaji and Aashish Gupta, “With COVID-19, India Experienced Its Greatest Mortality Crisis Since Independence”, 5 October 2021, https://science.thewire.in; Soutik Biswas, “Why India’s Real Covid Toll May Never Be Known”, 5 May 2022, https://www.bbc.com.
- “Tuberculosis”, WHO, https://www.who.int; “India Has Maximum Cases Of Tuberculosis In The World: WHO Report”, 9 November 2023, https://www.ndtv.com.
- Ankur Kalra et al., “The Burgeoning Cardiovascular Disease Epidemic in Indians – Perspectives on Contextual Factors and Potential Solutions”, 10 February 2023, https://www.thelancet.com; “‘India is Now the Chronic Heart Disease Capital of the World’ Warns CSI”, 30 September 2022, https://health.economictimes.indiatimes.com.
- “Diarrhoea in Children Under 5 More Prevalent in Rural India: NFHS-5”, 14 January 2021, https://www.downtoearth.org.in; “Diarrhoea Remains a Leading Killer of Young Children, Despite the Availability of a Simple Treatment Solution”, January 2024, https://data.unicef.org.
- Domestic General Government Health Expenditure (% of GDP), World Health Organisation, https://www.who.int; and Domestic General Government Health Expenditure (% of GDP), World Development Indicators, World Bank, https://databank.worldbank.org.
- Ibid.
- National Health Policy 2015: Draft, Ministry of Health and Family Welfare, 2014, p. 12, https://www.indiaspend.com.
- Economic Survey 2020–21, pp. 156, 159.
- Source: Domestic General Government Health Expenditure Per Capita (current US$), http://databank.worldbank.org.
- National Health Policy 2015: Draft, op. cit., p. 3.
- Ibid., p. 12.
- Ibid., p. 15.
- “Exclusive – Modi Government Puts Brakes on India’s Universal Health Plan”, 27 March 2015, https://www.business-standard.com; Apurva Vishwanath, “Supreme Court Tells Centre to Take Call on National Health Policy”, 14 September 2016, https://www.livemint.com; Amit Sengupta, “A Year of Apathy Towards Public Health Services, 25 December 2016, https://peoplesdemocracy.in.
- National Health Policy, 2017, Ministry of Health and Family Welfare, p. 5, https://main.mohfw.gov.in.
- “PM Modi Calls for Accessible, Affordable Healthcare for All Indians”, 13 September 2024, https://www.medicalbuyer.co.in.
- “PM Narendra Modi Promises Affordable Healthcare for All”, 27 January 2019, https://www.livemint.com.
- “‘Healthcare for All Creatures’: PM Modi Pitches for ‘One Earth One Health’”, 6 March 2023, https://www.hindustantimes.com.
- “India Rubbishes Lancet Report, Says Spending on Healthcare Is at All-Time High”, 15 April 2024, https://timesofindia.indiatimes.com.
- “Statement 27: Expenditure on Medical and Public Health and Family Welfare – As per cent of Aggregate Expenditure”, State Finances: A Study of Budgets of 2023–24, RBI, December 2023, https://rbidocs.rbi.org.in.
- The Economic Survey of the Government of India claims that the total General Government (Centre and States combined) public expenditure on health has increased from 1.2 percent of GDP in 2014–15 to 1.9 percent of GDP in FY22 and FY23. But the footnote to the data says that health expenditure includes spending on water and sanitation. The budget of the Department of Drinking Water and Sanitation this year is Rs. 77,391 crore. Excluding this, the actual General Government expenditure on health for India would not be more than 1.2 percent of GDP. Note that the WHO and WB also estimate India’s general government expenditure on health to be not more than 1.2 percent of GDP, as pointed out above in this article.
- “India’s Elections: Why Data and Transparency Matter”, The Lancet, 13 April 2024, https://www.thelancet.com.
- See: Indian Public Health Standards, National Health Mission, https://nhm.gov.in.
- All figures from: Rural Health Statistics 2021–22, Ministry of Health and Family Welfare, https://hmis.mohfw.gov.in.
- Ibid.
- Ibid.
- The data for functioning health centres is from RHS 2021–22, op. cit. The percentage of health centres functioning as per IPHS guidelines in 2019–20 is calculated from data given in Tables 38, 42 and 44, Rural Health Statistics 2019–20, Ministry of Health and Family Welfare, https://hmis.mohfw.gov.in. We assume that this percentage has remained the same in 2021–22.
- “Target of Starting 1.5 lakh Ayushman Bharat Health and Wellness Centres Achieved: Govt”, 30 December 2022, https://www.livemint.com.
- Shubhangi Derhgawen, “The Faltering Promise of Modi’s ‘Temples of Health’: Healthcare Centres That Fail the Poor, Censured by Govt’s Own Auditor”, 16 October 2024, https://article-14.com; Ramya Kannan, “Of Killer Hospital Tragedies, and Handling Cancers and Tuberculosis”, 11 October 2023, https://www.thehindu.com.
- https://qps.nhsrcindia.org/sites/default/files/2024-04/DO_Renaming%20AB-HWCs%20as%20Ayushman%20Arogya%20Mandir_25%2011%2023.pdf
- “Urban Health Mission to Cover 7.75 Crore People”, 2 May 2013, http://www.thehindu.com.
- The Union Budget papers give allocation for NURM for the years 2015–16 to 2021–22 only. For 2014–15, the allocation for NURM is from a reply given in the Lok Sabha on 31 March 2017.[National Urban Health Mission, Department of Health and Family Welfare, Lok Sabha Unstarred Question No. 5060, To be Answered on 31 March 2017, Digital Sansad, https://sansad.in.]
- All figures from: Rural Health Statistics 2021–22, op. cit.
- Data from: National Health Profile 2022, p. 406, https://www.cbhidghs.nic.in.
- Estimated using population for 2022 given in National Health Profile 2022, ibid.
- “India Needs Additional 2.4 Million Hospital Beds to Reach Recommended Ratio: Report”, 23 November 2023, https://www.millenniumpost.in.
- Estimated from the news report: “India Needs Additional 2.4 Million Hospital Beds to Reach Recommended Ratio: Report”, ibid. Total deficit of hospital beds = 23.46 lakh (taking population for 2022 to be 137.98 crore). Assuming half of this to come from public sector, this works out to 11.7 lakh.
- We have included both NHM in the Department of Health and Family Welfare, and NHM-AYUSH, in the NHM budget. From this, we deduct the allocation for ‘Human Resources for Health and Medical Education’ (a sub-head under NHM) as this is for upgrading / building hospitals in States (from 2021–22 onwards, this is excluded from the NHM budget). For the years 2023–24 and 2024–25, we add to the NHM budget: ‘Strengthening of State Drug Regulatory System’ and ‘Tertiary Care Programme’. These two sub-heads were earlier a part of NHM, but are excluded from NHM in these two years.
- For calculating this, we have combined the following three heads: (i) budget allocation for building new elite AIIMS like institutes and upgrading government medical colleges (this has been deceptively named Pradhan Mantri Swasthya Suraksha Yojana or PMSSY); (ii) budget allocation for ‘Human Resources for Health and Medical Education’ (this scheme is for upgrading district hospitals and building new medical colleges in States; and (iii) ‘Establishment Expenditure of New AIIMS’ (this new sub-head has been added since 2023–24 budget.
- This is well brought out in this case study of the situation in AIIMS, Delhi: Bilal Kuchay, “Is India’s Healthcare Policy Failing Its People?”, https://www.trtworld.com
- Banjot Kaur, “Despite What He Says, Not a Single AIIMS Set Up Under PM Modi Is ‘Fully Functional’ Yet”, 15 March 2023, https://thewire.in; Banjot Kaur, “Health Ministry Fails to Spend Rs. 8550.21 Crore – More Than ‘Establishment Cost of New AIIMS’”, 30 July 2024, https://thewire.in.
- Update on Ayushman Bharat Cards, 2 August 2024, https://pib.gov.in.
- “Indians Sixth Biggest Private Spenders on Health Among Low-Middle Income Nations”, May 8, 2017, https://archive.indiaspend.com; “Evolution and Patterns of Global Health Financing 1995–2014”, April 19, 2017, https://www.thelancet.com. Since then, the Centre claims that out-of-pocket expenses of Indians as a percentage of total health expenditure has fallen to less than 50 percent, but this is doubtful as we discuss later in this article.
- Soham D. Bhaduri, “A Health Scheme Sans Clout”, 10 March 2020, https://www.thehindu.com.
- Banjot Kaur, “Treatment for the Dead, Discharge Before Surgery and the Many Problems of Ayushman Bharat”, 10 August 2023, https://thewire.in.
- Economic Survey 2020–21, Vol. 1, p. 163.
- Cited in: Banjot Kaur, “Treatment for the Dead, Discharge Before Surgery and the Many Problems of Ayushman Bharat”, op. cit.
- “Budget 2019: Ayushman Bharat Gets Rs 6,400 Crore, But to Benefit Private Sector”, 1 February 2019, https://thewire.in.
- “In the Wake of Ayushman Bharat Come Sops for Private Hospitals”, 9 January 2019, https://thewire.in; “Only a Strong Public Health Sector Can Ensure Fair Prices and Quality Care at Private Hospitals”, 28 March 2019, https://scroll.in; Shailender Kumar Hooda, “With Inadequate Health Infrastructure, Can Ayushman Bharat Really Work?”, 26 November 2018, https://thewire.in.
- National Health Accounts Estimates for India (2019–20) Released, PIB Press Release, 25 April 2023, https://pib.gov.in.
- Out-of-Pocket Expenditure as Percentage of Current Health Expenditure (CHE) (%): Data by Country, Global Health Observatory data repository, WHO, https://apps.who.int.
- Indranil, “State of Health Financing in India: The Myth of OOP Reduction”, in State of Finance in India Report, 2022–23, https://www.cenfa.org; Mampi Bose, “The Illusion of India’s Improving Public Healthcare”, 1 December 2023, https://idronline.org.
- Asmi Sharma, “The State of Welfare: India’s Budget 2024–25”, 2 August 2024, https://idronline.org.
- Indranil, “State of Health Financing in India: The Myth of OOP Reduction”, op. cit.
- Sarwal R. et al., Investment Opportunities in India’s Healthcare Sector, NITI Aayog, March 2021, https://www.niti.gov.in.
- Health Insurance for India’s Missing Middle, NITI Aayog, October 2021, https://www.niti.gov.in.
- Swagata Yadavar, “More Indians Die of Poor Quality Care Than Due to Lack of Access to Healthcare: 1.6 Million”, 6 September 2018, https://www.indiaspend.com.
- “Medical Tourism – How India Is Leading the Game”, 14 July 2024, https://timesofindia.indiatimes.com.
- Medical Tourism in the Country, 25 July 2024, https://pib.gov.in.
(Neeraj Jain is a social–political activist with an activist group called Lokayat in Pune, and is also the Associate Editor of Janata Weekly, a weekly print magazine and blog published from Mumbai. He is the author of several books, including ‘Globalisation or Recolonisation?’ and ‘Education Under Globalisation: Burial of the Constitutional Dream’.)



