Minister of State for Health and Family Welfare Bharati Pravin Pawar recently claimed that India’s doctor-population ratio exceeds the World Health Organization’s recommendation. But factors such as skewed proportion of health workforce across states, rural-urban and public-private sectors, and lack of a live register for practicing doctors highlighted how the numbers shown in the Parliament do not represent the full picture.
While claiming that there is no dearth of doctors in the country, Pawar told Rajya Sabha on July 26 that, “There are 13,08,009 allopathic doctors registered with the State Medical Councils and the National Medical Commission [NMC] as on June 2022. Assuming 80% availability of registered allopathic doctors and 5.65 lakh AYUSH doctors, the doctor-population ratio in the country is 1:834 which is better than the WHO standard of 1:1000.”
Factchecker referred to official data on public health and spoke to experts to provide context to this claim, which has been made several times in Parliament.
Ayush doctors
Popularly, this number is broken down into a ratio of 1 doctor to 3 nurses, or 1 doctor to 2 nurses and 1 Auxiliary Nurse and Midwife, explained Dr T Sundararaman, former executive director of the National Health Systems Resource Centre and former Dean at School of Health System Studies at TISS, Mumbai. This translates to about 10 doctors per 10,000 population and 1 per 1,000.
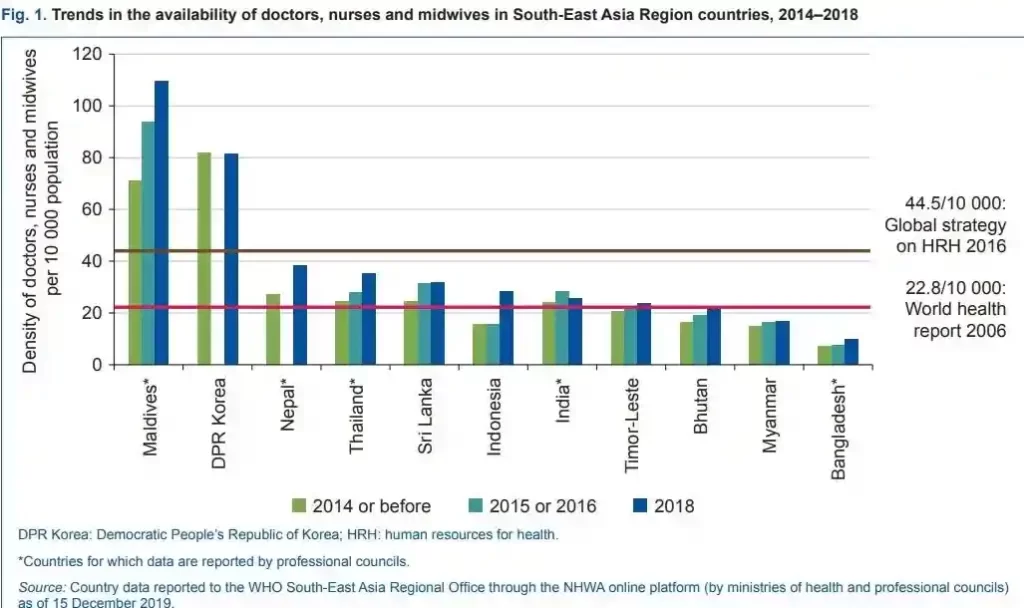
According to a 2021 report by the World Health Organization, India was way below the 44.5:10,000 ratio till 2018, and was just above the 2006 standard of 22.8 healthcare workers per 10,000 population.
Moreover, while Pawar included the 5.65 lakh Ayush – ayurveda, yoga and naturopathy, unani, siddha – doctors in the calculation, Dr Sundararaman said practitioners of traditional medicine are usually not included in this global formula.
Dr KR Antony, Former Health and Nutrition Specialist for the United Nations Children’s Fund, and former director, State Health Resource Centre, Chhattisgarh, echoed this view. He said the World Health Organization formula is “globally applicable for comparative assessment” and so in India, “Ayush doctors cannot be treated at par with MBBS doctors in the total figure.”
He added that focussing on a blanket nationwide ratio without looking at nuance and disaggregated data is misleading.
Gaps in data
The Ministry of Health and Family Welfare claims that 80% of registered allopathic doctors practice medicine in India and the rest of the 20% have either died, retired, stopped practice, never practiced or migrated.
But a 2021 study, led by Anup Karan, additional professor at the Indian Institute of Public Health, found that the density of active health workforce in India is just a little over one-fourth of the World Health Organization’s recommended threshold of 44.5 skilled health workers per 10,000 population. They found that the shortage for midwives and nurses is much more severe.
“A substantial proportion of active health workers were found not adequately qualified on the one hand, and on the other more than 20% of qualified health professionals are not active in labour markets,” read the study, which analysed two sources of data: National Health Workforce Account 2018 and Periodic Labour Force Survey 2017-’18.
One reason for this is that the National Medical Commission, which is referred to by Dr Pawar for the doctor-population ratio, does not maintain a live registry of doctors. The Indian Medical Registry fails to accurately account for migration of doctors – both within India and internationally – death and retirement, leading to double counting and an inflation of figures.
Dr Gagandeep Kang, virologist and Professor at Christian Medical College, Vellore, told FactChecker that students who have completed their MBBS degree can enrol themselves in the register maintained by the state medical councils and the National Medical Commission.
This means that not only is there no de-registration process for a doctor after their death or retirement, but also there is no account of doctors who might be teaching, involved in research or lab work, and other allied occupations other than actively practicing medicine.
The latest National Sample Survey Organisation Health Workforce Survey 2017-18, which provides another estimate of the doctor population in India, highlighted that 27% individuals with a qualification in medicine – graduation or above – are not active in the labour market, while approximately 4% are unemployed and looking for jobs.
So, according to the survey, around 69% of doctors, including the ones who might be engaged in teaching or research, are available to treat patients. “The NSSO projections show that the ministry’s presumption of an 80% active physician workforce appears somewhat inflated,” said Dr Soham Bhaduri, Chief Editor of the peer-reviewed journal The Indian Practitioner and health policy expert.
Shortfall in rural areas
While the Centre claimed in Parliament that India exceeded the World Health Organization’s prescribed standard of doctor-population ratio, the Rural Health Statistics 2021 released by the health ministry showed that across rural and urban areas, there is a 7% shortfall of doctors at Primary Health Centres and a 57% shortfall of doctors at Community Health Centres.
For a Primary Health Centre, which is the first contact point between the village community and a medical officer, the norm is one doctor or medical officer per centre. A Community Health Centre, which acts as a referral point for four Primary Health Centres, is to be manned by at least four specialist doctors – a surgeon, a physician, a gynaecologist, and a paediatrician.
Almost two-third of the country’s population resides in rural areas and yet only 33% of the total health workers and 27% doctors are available in rural areas, revealed the 2021 statistics.
Even though the number of health centres has increased in rural areas, the shortage of doctors in Community Health Centres has risen from 45% in 2005 to 80% in 2021, and has remained constant in Primary Health Centres at 4.3%. In urban areas, the shortfall at Primary Health Centres is 9.8% and at Community Health Centres it is 34%.
This is mainly the result of “an archaic policy and inefficiency in recruitment”, said Dr Sundararaman. In most states, the doctors in rural health centres are appointed on a contract, with no hardship allowance and little incentives.
The distribution of the health workforce across states is also highly skewed as some states have surplus doctors and some experience an inadequacy. Nine states and Union Territories face a shortage of doctors at Primary Health Centres in rural areas. In urban areas, the corresponding number is eight.
For Community Health Centres, all states experience a shortfall in specialist doctors in rural areas. Out of the 21 states where urban Community Health Centres exist, 17 states reel under such a shortage.
Patients prefer private sector
In India, healthcare is dominated by private healthcare providers. In the early 1950s, the share of the private sector was 8% of the total healthcare market which has now risen to 70%. Almost two-third of all doctors are employed in the private sector. The distribution of doctors across public and private clinics is clearly uneven.
“When talking about a country’s health status, and availability of doctors, the skewed ratio of dispersion of public-private medical practitioners in rural versus urban areas is a factor that needs to be considered,” said Dr Antony.
For private healthcare settings, the cost of hospitalisation is seven times the cost in government hospitals, revealed the National Sample Survey Household Social Consumption statistics 2017-’18. Only 14% of the rural population and 19% of the urban population reported that they had health expenditure coverage.
Even then, only 30% of people overall went to a government hospital to seek treatment for an illness, 43% went to a private doctor or clinic, 23% went to a private hospital and 4% went to charity-based hospitals. Every four out of 10 people chose a government hospital for in-patient hospitalisation.
“A large chunk of doctors work exclusively in the private sector, and dual practice among government doctors is rampant. The latter is well known to be fuelling physician absenteeism in our government health centres which significantly erodes any gains obtained from having adequate, or even excess doctors,” said Dr Bhaduri.
Choice of the private sector, despite higher prices, is essentially guided by the absence of doctors and healthcare workers, along with quality constraints of the public sector, found a 2019 research paper published in the International Journal for Healthcare Management.
In order to arrive at a more accurate doctor-population ratio, it’s important to plug these loopholes and ascertain the number of doctors actually seeing patients, Dr Kang concluded.
FactChecker wrote to Dr Pawar’s office requesting for a clarification on their statement considering the above-mentioned factors and also tried calling her, but had received no response by the time of publishing. If and when we receive a response, it shall be updated here.
(Courtesy: FactChecker.in, a dedicated fact-checking initiative of IndiaSpend that examines statements and assertions by prominent figures in public life for both accuracy and context.)